Bladder cancer originates from the lining of urinary bladder which is an organ in your pelvic area that stores urine. Bladder cancer more commonly affects older adults, though it can occur at any age.
Majority of bladder cancers are diagnosed at an early stage — when bladder cancer is highly treatable. However, even early-stage bladder cancer is likely to recur. For this reason, regular follow ups after treatment of bladder cancer is necessary to look for bladder cancer recurrence.
The treatment ,prognosis and follow up of urinary bladder cancer depends on stage (depth of the wall involved by cancer) and grade of the disease(high grade vs low grade). Superficial (non muscle invasive) and low grade tumors may be treated with endoscopic surgery through the normal urinary passage which is called TURBT. TURBT is also the first step in treatment even for muscle invasive bladder cancer which then need removal of complete bladder surgically (Radical cystectomy) once muscle invasion is confirmed on TURBT. Radical cystectomy further involves creation of alternate passage for urine(Urinary diversion). Sometimes radical cystectomy is also indicated for high risk non muscle invasive bladder cancers.

Signs and symptoms
Clinical manifestations of bladder cancer are as follows:
- Painless gross hematuria which means visible blood in urine – Approximately 80-90% of patients; classic presentation. It is important that even a single episode of hematuria (blood in urine) is not ignored.
- Irritative bladder symptoms (eg, dysuria, urgency, frequency of urination) – 20-30% of patients.
- Pelvic or bony pain, lower-extremity edema, or flank pain – In patients with advanced disease.
- Palpable mass on physical examination – Rare in superficial bladder cancer.
Causes
- It’s not always clear what causes bladder cancer. Bladder cancer has been linked to smoking, a parasitic infection, radiation and chemical exposure.
Risk factors
Factors that may increase your risk of bladder cancer include:
- Smoking.Smoking cigarettes, cigars or pipes may increase your risk of bladder cancer by causing harmful chemicals to accumulate in your urine. When you smoke, your body processes the chemicals in the smoke and excretes some of them in your urine. These harmful chemicals may damage the lining of your bladder, which can increase your risk of cancer.
- Increasing age.Your risk of bladder cancer increases as you age. Bladder cancer can occur at any age, but it’s rarely found in people younger than 40.
- Men are more likely to develop bladder cancer than women are.
- Exposure to certain chemicals.Your kidneys play a key role in filtering harmful chemicals from your bloodstream and moving them into your bladder. Because of this, it’s thought that being around certain chemicals may increase your risk of bladder cancer. Chemicals linked to bladder cancer risk include arsenic and chemicals used in the manufacture of dyes, rubber, leather, textiles and paint products..
- Chronic or repeated urinary infections or inflammations (cystitis), such as might happen with long-term use of a urinary catheter, may increase your risk of a squamous cell bladder cancer. In some areas of the world, squamous cell carcinoma is linked to chronic bladder inflammation caused by the parasitic infection known as schistosomiasis.
- Personal or family history of cancer.If you’ve had bladder cancer, you’re more likely to get it again. If one or more of your immediate relatives have a history of bladder cancer, you may have an increased risk of the disease, although it’s rare for bladder cancer to run in families. A family history of hereditary nonpolyposis colorectal cancer, also called Lynch syndrome, can increase your risk of cancer in your urinary system, as well as in your colon, uterus, ovaries and other organs.
How is Urinary Bladder Cancer diagnosed?
Tests and procedures used to diagnose bladder cancer may include:
- Cystoscopy. Cystoscopy is an endoscopic examination in which a cystoscope is introduced through normal urinary passage to examine the inside of urethra and urinary bladder to look for any growth/abnormal areas. Cystoscopy may be done under local anaesthesia using a flexible cystoscope or ot may be done under anaesthesia to remove the growth when we already know from other tests that growth is present in bladder. This procedure is then called transurethral resection of bladder tumor (TURBT).
- Biopsy. During cystoscopy, a sample of abnormal area or growth is taken and sent for microscopic examination. Sometimes even in absence of any abnormal area or growth a biopsy may needed. This usually happens when patient presents with malignant(cancerous) cells on urine cytology (urine test) but other imaging (such as ultrasound / Contrast CT scan) show no evidence of growth in urinary tract.
- Urine cytology. A sample of your urine is analyzed under a microscope to check for cancer cells in a procedure called urine cytology.
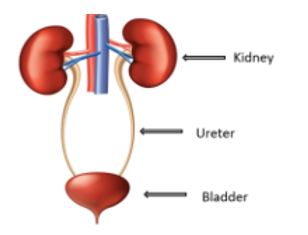
- Imaging tests. Imaging tests allow your doctor to examine the structures of your urinary tract. Ultrasound is most common first test used. Tests to highlight the urinary tract sometimes use a dye, which is injected into a vein before the procedure. A computerized tomography (CT) scan is a type of X-ray test that allows your doctor to better see your urinary tract and the surrounding tissues.
What are the treatment options for urinary bladder cancer?
Treatments and drugs
Your treatment options for bladder cancer depend on a number of factors, including the type and stage of the cancer, your overall health, and your treatment preferences. Discuss your options with your doctor to determine what treatments are best for you.
Treatment of superficial bladder cancer
Superficial bladder cancer is a cancer which has not invaded the muscle wall of the bladder and is confined to the inner lining of the bladder. It may refer to as either Ta, T1 or Tis (also known as Carcinoma in situ or “CIS”). After the initial TURBT or biopsy in case of CIS, the subsequent treatment in these cases may involve observation with regular follow up with cystoscopy examinations of the bladder, instillation of medications in the bladder, or in certain cases, surgical removal of the bladder (“radical cystectomy”). The follow up and further treatment of these superficial (non muscle invasive) bladder tumors depend on their tendency to recur or progress. This is determined by features which classify a particular tumor to be a low risk, intermediate risk of high risk tumor.

Small low grade, superficial bladder cancers may not require aggressive management after the initial TURBT and may be simply followed up by doing repeated cystoscopy examinations at regular intervals (usually every 3 to 6 months for the first year and then at increasing intervals). Recurrent tumors may be surgically removed or fulgurated (“burnt out”) with special instruments passed through the cystoscope. It is very important to note that 30-40% of these tumors tend to recur and these recurrences may not be associated with any symptoms. Hence, it is imperative to stick to a regular follow up protocol to ensure that the disease does not go out of control. It has also been shown that a single dose of a chemotherapy medication (e.g. Mitomycin C) put inside the bladder immediately after a TURBT can decrease the chances of recurrence within the first 2 years after surgery. It should be noted that CIS, although superficial is a high grade disease and should be managed as other high grade tumors.
High grade, larger, multiple or recurrent superficial bladder cancers require additional treatment after the initial TURBT. This most commonly includes intravesical instillation of BCG (Bacille Calmette Guerin, which is commonly used for vaccination against human tuberculosis ). BCG ia available in powder form which is usually dissolved in 50 ml of normal saline and is instilled into the bladder in the form of a solution using a catheter placed in the urinary passage. It is a form of immunotherapy and acts by stimulating the immune system of the body to act against the cancerous bladder cells and prevent their growth and development. BCG has been shown to decrease the chances of recurrence of bladder cancer as well as progression (its invasion into the muscle layer of the bladder). However, since it is only partially effective in reducing recurrence and progression, a regular follow up with cystoscopy is a must to keep a check on disease status. BCG therapy has two phases: an induction phase which means 6 initial doses at weekly intervals followed by a “maintenance” phase which is usually recommended for atleast 1 year but may last as long as 3 years.
Patients, who do not respond to BCG treatment, recur in spite of treatment or those who have medical issues which preclude the use of BCG, may require other forms of treatment. These include bladder instillation of immunotherapy agents or chemotherapy medicines like Valrubicin, Mitomycin C, Epirubicin or Adriamycin. More likely these patients are candidates for Radical Cystectomy as these medications are not as effective as BCG and help only a small minority of patients who have not responded to BCG.
In some patients who have an aggressive form of high grade superficial bladder cancer or variant histolgy such as micropapillary are also candidates for Radical cystectomy which entails removal of the bladder and prostate (uterus in females) and creating an alternate pathway for urine using parts of the intestine. The details and various diversion are explained in management of muscle invasive bladder cancer.
Surveillance for bladder cancer after treatment of superficial(non muscle invasive) bladder tumors
Patients diagnosed and treated with superficial bladder cancer need to be followed up regularly to detect recurrences and treat them effectively. A typical follow up protocol includes again depends on whether the tumor was low, intermediate or high risk
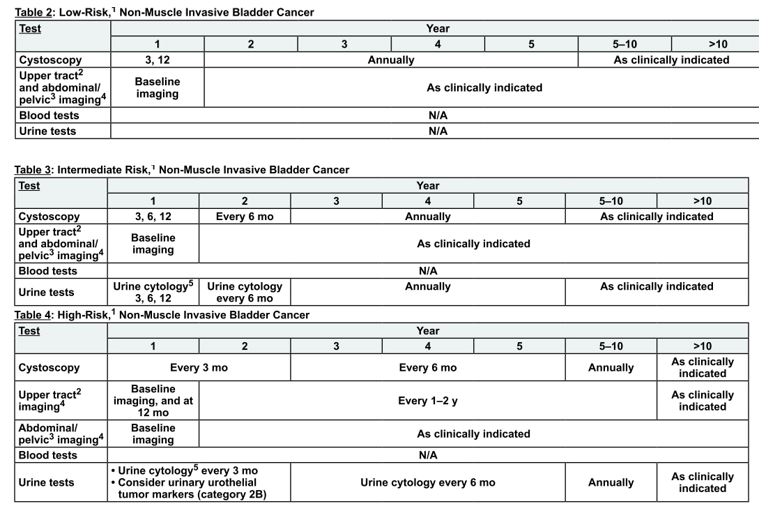
Cystoscopy and cytology detects recurrence in the bladder itself while CT/IVU is used to detect a tumor in the kidneys and ureters. Patients with bladder cancer are more likely to get “upper tract” tumors, which arise from the inner lining of these organs and share a common origin with bladder tumors
Treatment of muscle-invasive bladder cancer
The standard and most effective treatment for muscle invasive bladder cancer is the surgical removal of the bladder (Radical Cystectomy) and diversion of the urine using intestinal segments.The procedure involves removal of the bladder, prostate, seminal vesicles and the fatty tissue around the bladder through an incision made in the abdomen. The surgery also includes removal of lymph nodes in the pelvis on both sides of the bladder to detect their involvement with the cancer. This helps in accurate staging and deciding further management after surgery including the need for chemotherapy. It has been shown that patients who undergo a thorough lymph node dissection have a better chance of cure as compared to patients who either do not receive one or undergo a less extensive dissection.
Radical cystectomy can be performed via open surgery, laparoscopy or with robotic assistance. All the three modalities have similar oncological outcomes(cancer control rates). However, minimal invasive approaches( laparoscopic and robotic) are advantageous in terms of decreased blood loss during the surgery and hence decreased need for blood transfusions, lesser incidence of wound infection, lesser post operative pain and early recovery. Robot also has additional advantage of permitting an enhanced magnification of the surgical field with 3 dimensional vision which helps to enhance surgical precision. Technologically advanced robotic instruments with endowrist function and increased maneuverability paricularly in narrow pelvic area is a boon for the surgeon to provide good results. However, experience of an individual surgeon in a particular approach is an important factor in decision regarding selection of the approach for surgery.
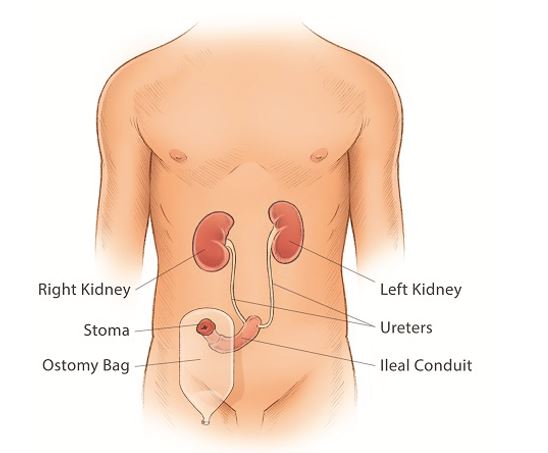
Urinary Diversion(Creating an alternate pathway for urine): Once the bladder has been removed, the urine needs to be diverted. This requires the use of segments of the intestine which are still connected to their blood supply but have been disconnected from the gastro-intestinal tract (rest of the intestine whose continuity has been reestablished by anastomosis.
- Ileal conduit is the most extensively used form of urinary diversion. It is also the simplest and the least time consuming form of diversion and has the least chances of complications in the short and long term. This entails the use of an intestinal segment, one end of which is connected inside the body to the ureters that drain urine into it from the kidneys, while the other end is brought out to the level of the skin and is covered by an external appliance (a “urostomy bag”). The urine from the kidneys continuously drains into the bag through the ureters and the “ileal conduit”. The bag can be emptied at regular intervals or when it is nearly full by opening a tap-like attachment at the lower end of the bag. The major advantage of this procedure is that is relatively straightforward to perform with least chances of complications. The disadvantages include the need to wear a bag all the time and the resultant negative impact that may occur on body image.
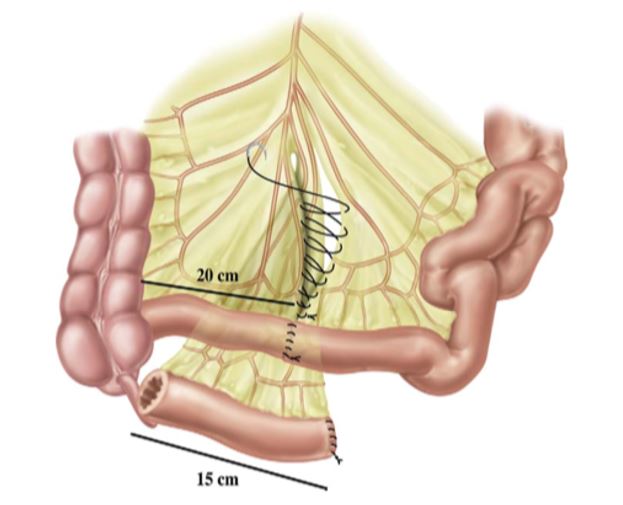
The isolated ileal segment to be used as a conduit is lying below the digestive anastomosis, and the mesentery window of the ileo-ileal anastomosis is sutured.
- Orthotopic neobladder entails the creation of a new bladder (“neobladder”) with the help of an intestinal segment and connecting it to the natural urinary passage so that a person may be able to pass urine “more normally”. The major advantage of this procedure is that it avoids the need to wear a bag and the patient can pass urine in a more natural fashion. However, this is a more difficult procedure with a longer recovery period and may lead to some short term and long term complications including persistent urinary leakage and inability to pass urine requiring the use of self intermittent catheterization (passage of a tube into the urinary passage to empty the bladder). Some senior patients and those with certain medical conditions that affect the function of the kidneys or impair their ability to self catheterize may be best served by the ileal conduit rather than the neobladder.
Options for patient not fit/unwilling for Radical Cystectomy
- Radical cystectomy (open, laparoscopic or robot assisted) combined with one of the urinary diversions is the “gold standard” for the treatment of muscle invasive and selected cases of high grade superficial bladder cancer. Certain patients, however, may be unfit or unwilling to undergo this surgery. These patients can often undergo a combination of extensive TURBT + Chemotherapy + Radiation in an attempt to cure or control the disease without the need to remove the urinary bladder surgically. Most experts believe that this regime may not be as effective as a radical cystectomy but can be used as an option in unfit/unwilling patients. Radiation to the bladder can however lead to its own set of problems and complications including radiation damage to the bladder and rectum giving rise to bleeding and irritative symptoms (“radiation cystitis” and “radiation proctitis”).
Chemotherapy for bladder cancer
Chemotherapy in bladder cancer patients may be considered in three situations
- Patients who are diagnosed with metastatic bladder cancer (M stage – M1), i.e. cancer, which has spread to other parts of the body, are usually treated with chemotherapy.
- After surgery (Adjuvant chemotherapy): chemotherapy may be used in cases of locally advanced bladder cancer (T stage – T3 and above and/or N stage – N1 and above) in an attempt to decrease the chances of the cancer coming back after radical cystectomy.
- Before surgery (Neoadjuvant chemotherapy) : Chemotherapy before Radical Cystectomy may be given in an attempt to improve the results of surgery and decrease the size of the tumor. Neoadjuvant chemotherapy may not be considered if a patient of muscle invasive bladder cancer has decreased renal function or raised creatinine.
- Chemotherapy regimens include:
- MVAC regimen . It is a combination of 4 medications given in cyclical form and include (M–Methotrexate,V – Vinblastine, A – Adriamycin (Doxorubicin) and C – Cisplatin). Adriamycin has some cardiotoxicity and may be avoided in heart patients.
- GC regimen: An alternative regimen is a combination of two medications, Gemcitabine and Cisplatin. This is increasingly being used nowadays.
It is important to note that Cisplatin is the main medication in all these regimens and patient should have normal kidney function for it to be used.
Prognosis for bladder cancer
Stage and grade are the most important factors that impact the prognosis of bladder cancer after treatment. Lower the Stage and Grade, better the outcome for the patient. Other factors such as number, size, pattern of recurrence, response to initial treatment like BCG, coexistent carcinoma in situ and certain genetic mutations also play a role.
Recurrence is common in urothelial cancers (20-30% in 5 yrs for low risk superficial tumors and 60-70% in 5 yrs for high risk tumors). Progression to muscle invasive however is rare in low risk superficial cancers. On the other hand, high risk superficial tumors are much likely to invade into the deeper layers with progression rates of 17% and 45% at 1 and 5 years.
After radical cystectomy, survival depends mostly on the stage of the disease. 5-year disease specific survival (i.e. the percentage chance that an individual will NOT die because of bladder cancer in the first 5 years after surgery) for various stages after a radical cystectomy is as follows.
- T2, N0: 70 – 80%
- T3, N0: 40 – 50%
- T4, N0: 25 – 30%
- N+ (patients with lymph node involvement): 15 – 20%
5-year survival is rare in patients with metastatic disease despite chemotherapy. It is important to note that these are statistics compiled for large groups of patients. Every individual patient is different from the others and may have outcomes starkly different from those mentioned in the average analysis above.
Prevention of Bladder Cancer
The best way to prevent bladder cancer is to avoid exposure to agents that cause the disease. People who don’t smoke are 3 – 4 times less likely to get bladder cancer as compared to smokers. Continuing to smoke after the diagnosis of bladder cancer portends a poorer outcome and increases the chance of the disease coming back after treatment. Avoidance of occupational exposure to cancer causing chemicals such as aniline dyes may also be important. Despite research in this area no medication or dietary supplement has been conclusively demonstrated to decrease the risk of bladder cancer in normal individuals.
Keypoints