How is Robotic Radical prostatectomy performed?
Robotic Radical Prostatectomy, also known as Robotic surgery for prostate cancer or da Vinci® Prostatectomy is a minimally invasive surgery that is now the preferred approach for removal of the prostate in those diagnosed with organ-confined prostate cancer. The da Vinci Prostatectomy may be the most effective, least invasive prostate surgery performed today. Though any diagnosis of cancer can be traumatic, the good news is that if your doctor recommends prostate surgery, the cancer was probably caught early. And, with da Vinci Prostatectomy, the likelihood of a complete recovery from prostate cancer without long-term side effects is, for most patients, better than it has ever been.
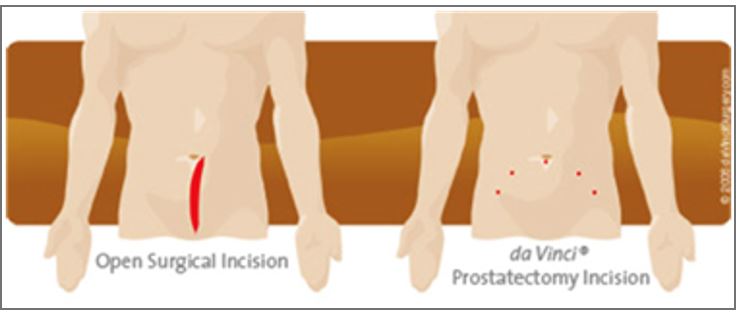
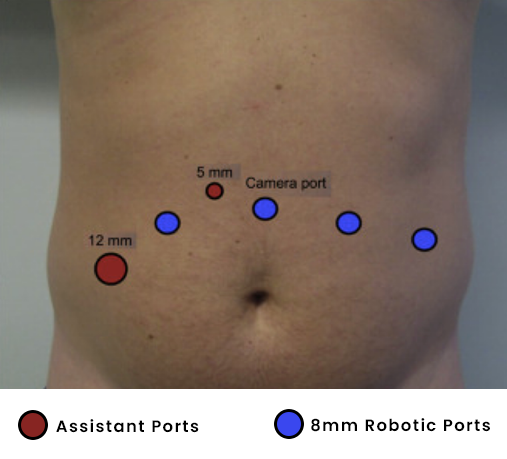
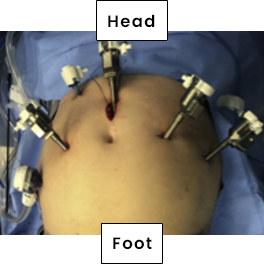
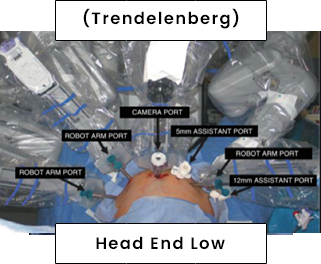
The operation is performed using the daVinci Surgical system and 3-D endoscopic and wristed instruments inserted through 5-6 small incisions across the mid-abdomen (See Figure below)
During the dVP, a telescopic lens is inserted into one of the small incisions. This provides a magnified 3-dimensional view of the delicate nerves and muscle surrounding the prostate, thus allowing optimal preservation of these vital structures. The cancerous prostate gland is dissected free from the bladder and urethra, and the bladder and urethra are sewn together without the surgeon’s hands ever entering into the patient’s body. The prostate is removed intact through one of the small incisions located at the lower abdomen to accommodate the size of the prostate. These small incisions are closed with absorbable suture.
What are the benefits of Robotic prostatectomy?
The da Vinci Surgical System enables surgeons to operate with unmatched precision and control using only a few small incisions. Recent studies suggest that da Vinci Prostatectomy may offer improved cancer control and a faster return to potency and continence.
The da Vinci Prostatectomy also offers these potential benefits:
- Significantly less pain and scarring
- Less blood loss
- Fewer complications
- A shorter hospital stay and faster recovery
- Faster return to normal daily activities
- Recent studies have shown early return to urinary continence after robotic radical prostatectomy.
As with any surgery, these benefits cannot be guaranteed, as surgery is both patient- and procedure-specific. While prostatectomy performed using the da Vinci Surgical System is considered safe and effective, this procedure may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits. If you are a candidate for prostate surgery, talk to your surgeon regarding Robotic Prostatectomy.
Robotic Radical prostatectomy
Preparation for surgery
Medications to Avoid Prior to Surgery
- If you are taking regular medication for any comorbidities, you might require to stop few of them preoperatively after consulting your surgeon/anesthetist or respective specialist. This typically involves stopping or altering the antiplatelet drugs(blood thinners). Do not stop any medication without contacting the prescribing doctor to get their approval).
Bowel Preparation• If your surgery is planned in morning hours, do not eat or drink anything after midnight the night before the surgery. Your surgeon will guide you regarding the planned time of surgery and will advise you to remain nil per mouth accordingly.
The Operation
Nerve-sparing Robotic radical prostatectomy is a well-established procedure and is performed with the assistance of an experienced and dedicated Robotic surgical team including nurses, anesthesiologists, operating room technicians, many of whom you will meet the day of surgery.
Robotic prostatectomy is performed through 4 to 5 less than 1-cm keyhole incisions across the mid abdomen (see port placement figure above). Through these small incisions, your surgeon uses fine robotic instruments to precisely dissect the prostate gland, seminal vesicles, and vasa deferentia from the urethra and bladder. These instruments are connected to robotic arms during docking of robot and then controlled by operating surgeon sitting on master console. (see section on what is Robotic surgery). This is in contrast to the conventional open radical retropubic prostatectomy where a lower midline abdominal incision is required for dissection and removal of the prostate gland.
Robotic telescope is inserted into camera port attached to robotic arm which then transmits 3D view of surgical field on master console. This provides the surgeon with excellent visualization and details of the prostate gland and the surrounding neurovascular structures, allowing for precise dissection of the prostate. Once the prostate gland is dissected free from the bladder, rectum, and urethra, it is placed in a small plastic bag and eventually removed by extending one of the keyhole incisions to accommodate the prostate. The bladder is sewn back to the urethra to restore continuity of the urinary tract. A Foley catheter is placed through the penis to drain the bladder and allow healing of the bladder-urethra connection. In addition, a small drain is placed around the surgical site, exiting one of the keyhole incisions.
The average length of operative time during robotic radical prostatectomy is 2.5 to 3 hours. However, it may vary from patient to patient depending on the size of the prostate gland, shape of the pelvis, weight of the patient, and presence of scarring or inflammation within the pelvis due to infection or prior abdominal/pelvic surgery. Blood loss during Robotic Radical prostatectomy is routinely less than 200 cc. Transfusions are rarely required. Donation of blood prior to surgery for autologous blood transfusion can be arranged if the patient desires but is not recommended.
Potential Risks and Complications
Although this procedure has proven to be very safe, as in any surgical procedure there are risks and potential complications. The safety and complication rates are similar when compared to the open surgery. Potential risks include:
Bleeding: Although blood loss during this procedure is relatively low compared to open surgery, a transfusion may still be required (in <1% of patients) if deemed necessary by your surgeon either during the operation or afterwards during the postoperative period.
Infection: All patients are treated with intravenous antibiotics, prior to the start of surgery to decrease the chance of infection from occurring within the urinary tract or at the incision sites.
Adjacent Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, pelvic musculature, and nerves could require further procedures. Transient injury to nerves or muscles can also occur related to patient positioning during the operation.
Hernia: Hernias at incision sites rarely occur. The larger keyhole incisions are closed under direct laparoscopic view.
Urinary Incontinence: As in open surgery, urinary incontinence can occur following Robotic prostatectomy, but often improves over time with the use of Kegel exercises, which help strengthen the urinary sphincter muscle. Recent studies have shown early return to urinary continence after robotic radical prostatectomy.
Erectile Dysfunction: Similar to open surgery, a nerve-sparing technique is attempted during robotic dissection of the prostate gland unless there is obvious involvement of the nerve tissue by tumor. The return of erectile function following prostatectomy is a function of the age of the patient, degree of preoperative sexual function, technical precision of the nerve-sparing technique, and time.
Urethrovesical Anastomotic Leakage: Transient small urinary leakage can occur rarely at the connection between the bladder and urethra and usually resolves without further intervention within a few days to up to a week. The urinary catheter will remain in place until the leakage has stopped.
WHAT TO EXPECT AFTER SURGERY?
During your hospitalization
Immediately after the surgery you will be taken to the recovery room, then transferred to your hospital room once you are fully awake and your vital signs are stable.
Hospital Stay: Length of hospital stay for most patients is 2-3 days.
Diet: You can expect to have an intravenous catheter (IV) in for 1-2 days. (An IV is a small tube placed into your vein so that you can receive necessary fluids and stay well hydrated; in addition, it provides a route to receive medication.) Most patients are able to tolerate liquid/soft diet the first day after surgery, and a regular diet the following day. Once on a regular diet, pain medication will be administered by mouth instead of by IV or shot.
Post-Operative Pain: Pain medication can be controlled and delivered by the patient via an intravenous patient-controlled analgesia (PCA) pump or by injection (pain shot) administered by the nursing staff. You may experience minor transient shoulder pain (1-2 days) related to the carbon dioxide gas used to inflate your abdomen during the robotic surgery.
Bladder Spasms: Bladder Spasms are commonly experienced as a moderate cramping sensation in the lower abdomen or bladder and are quite common after prostatectomy. These spasms are usually transient and often decrease over time. If severe, medications can be prescribed by your doctor to decrease the episodes of these spasms.
Nausea: You may experience transient nausea during the first 24 hours following surgery, which can be related to the anesthesia. Medication is available to treat persistent nausea.
Urinary Catheter: You can expect to have a urinary catheter (Foley) draining your bladder (which is placed in the operating room under anesthesia) for approximately 7-10 days after the surgery. It is not uncommon to have blood-tinged urine for a few days to a week after your surgery.
Pelvic Drain: The pelvic drain is placed in the operating room and drains the pelvic space around the bladder-urethra anastomosis. This drain is usually removed next day of surgery.
Incentive Spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections by using an incentive spirometry device (these exercises will be explained to you during your hospital stay). Coughing and deep breathing is an important part of your recuperation and helps prevent pneumonia and other pulmonary complications.
Ambulation: On the day after surgery, it is very important to get out of bed and begin walking with the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can expect to have SCD’s (sequential compression devices) along with tight white stockings on your legs to prevent blood clots from forming in your legs while you are lying in bed.
Constipation/Gas Cramps: You may experience sluggish bowels for few days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
What to expect after discharge from the hospital?
Pain Control: You can expect to have some incisional discomfort which is usually well tolerated. However rarely it may require pain medication for a few days after discharge and paracetamol should be sufficient upon returning home to control your pain.
Showering: You may shower at home. Your wound sites can get wet but must be padded dry.
Incision and suture: Your incisions will be closed with absorbable sutures both on and beneath the skin, which usually dissolves in 4-6 weeks.
Activity: Taking daily walks is strongly advised. Prolonged sitting or lying-in bed should be avoided and can increase your risk for forming blood clots in the legs as well as developing pneumonia. Climbing stairs is possible but should be limited. Driving should be avoided for at least 2 weeks after surgery. Most patients return to full activity an average of 3-4 weeks after surgery. Absolutely no heavy lifting (greater than 5 kgs) or exercising (jogging, swimming, treadmill, biking) for six weeks or until instructed by your doctor.
Medications: You can resume your usual medications after surgery including plain aspirin 75 mg but with the exception of other stronger blood thinners, which can increase the risk of bleeding. Your doctor will advise you on individual basis regarding the discharge medications.
Follow-up Appointment: Prior to discharge from the hospital, you will be given postoperative instructions by your surgeon.
In addition, you will be instructed on when to follow up in the office for removal of your Foley catheter (typically 7-10 days after the date of surgery).
Pathology Results: Pathology results are usually available approximately 7 days following surgery. These results will be reviewed with you in the office. Alternatively, you can contact your surgeon by phone or email at one week.
Long-term Follow-up: A prostate-specific antigen (PSA) test is drawn at one month following surgery. Patients are re-evaluated every 3-6 months. This can be easily accomplished over the telephone for patients who do not live close to the hospital.
Discharge Instructions
CATHETER CARE:
Your catheter is very important to allow healing of the bladder to the urethra. The catheter should drain your bladder continuously. It should not be put on tension at any time. If you feel pulling or tugging, this means that your catheter needs to be fastened higher up on your leg to allow for some slack on the catheter as you move and walk. Your surgeon should be notified immediately if the catheter stops draining completely or if it falls out.
The urine collection bag must be positioned at all times below the bladder for proper draining by gravity. Drain the bag before it gets too full as this will result in a backup of urine in the bladder. Although use of the larger collection bag is advised, a smaller leg bag is available and can be worn under clothing. The larger bag is required at night as the smaller bags are likely to fill up too quickly.
The tip of the penis may get sore from catheter irritation. Use plain soap and warm water to wash this area daily. You may use water-based lubricants (K-Y jelly) to prevent dryness and discomfort at the tip of the penis. A small amount of blood-tinged urethral secretions or even urine may leak around the catheter at the tip of the penis especially during bowel movements. This occurs due to mild straining and is completely normal.
It is common for your urine to turn pink or red-tinged as you become more active simply from the catheter rubbing against your bladder lining. If this occurs, reduce your walking and increase your fluid intake. It is permissible to bring the urine collection bag in the shower.
DIET: You may return to your normal diet immediately upon discharge from surgery. However, adhering to foods such as rice, soups, noodles and avoiding high fiber meals (e.g., vegetables such as celery) is advised as your intestines may take up to a week to recover from the surgery an anesthesia. Because of the raw surface in your bladder and urethra, alcohol, spicy foods and drinks with caffeine may cause some irritation or sense of the need to void despite the fact that the catheter is emptying the bladder. If these foods don’t bother you however there is no reason to avoid them in moderation. More importantly is to keep your urine flowing freely, drink plenty of fluids during the day (8-10 glasses). The type of fluids (except alcohol) is not as important as the amount. Water is best but juices, coffee, tea, soda are all acceptable.
ACTIVITY: Strenuous physical activity is to be restricted, especially during the first few weeks. During this time use the following guidelines:
- Walking 6-8 separate short walks a day is advised to prevent blood clots from forming in the legs or pneumonia in the lungs.
- Climbing stairs is permitted if necessary but should be taken slowly. Climbing stairs is otherwise not a necessary activity in terms of exercise.
- No lifting heavy objects (anything greater than 5 kgs).
- No driving a car and limit long car rides.
- No strenuous exercise for 4-6 weeks. Following this, patients can return to their normal activities of daily living.
BOWELS: Your bowels should return to normal after the surgery (over the course of few days) though pain medications can cause constipation and therefore should be discontinued as soon as tolerated. The rectum and the prostate are next to each other and any very large and hard stools that require straining to pass can cause bleeding in the urine. Use a mild laxative (e.g. milk of magnesium) or stool softener (e.g. syrup cremaffin or looz) as advised.
MEDICATION:You should resume your pre surgery medication unless told not to. Plain aspirin 75 mg can be taken but we recommend staying off higher dose aspirin or aspirin-containing products until after the catheter comes out and for at least 4 weeks following surgery (Your doctor will advise you regarding the medication on an individual basis). You will be given a prescription for pain pills (e.g., Paracetamol) for incisional discomfort. Most men following robotic prostatectomy rely only on Paracetamol at home and do not require narcotic pain medication. You will also be given a prescription for an antibiotic (e.g., fosirol sachet 3 gm) given on the day of catheter removal. You will also be prescribed an anticholinergic drug (Mirabegron 50 mg once a day) for 3 weeks after discharge to alleviate any bladder spasms which you may have as a result of indwelling catheter.
HYGIENE: You may shower or bathe as soon as you get home. Dab your incision sites dry following a shower and avoid heavy creams or ointments on your incisions. Keeping them dry and open to air is adequate.
PROBLEMS YOU SHOULD REPORT TO US:
- Fevers over 101 degrees Fahrenheit as this may be a sign of infection.
- Heavy bleeding or clots in the urine.
- Calf or thigh pain or swelling as this may be a sign of a blood clot.
- Difficulty breathing or chest pain as this may be a sign of a pulmonary embolus or heart attack.
- Skin rash or hives as these may be signs of potential medication reactions.
- Nausea, vomiting, diarrhea which may be a sign of infectious diarrhea (e.g., Clostridium difficile)
- Call immediately if your catheter stops draining completely or falls out.
FOLLOW-UP:The first postoperative appointment will be to remove the catheter, usually done at 1-2 weeks after surgery. Your surgeon will decide on the timing of this and this appointment will be arranged through the urology clinic). Most people will have some difficulty initially with urinary control at the time the catheter is removed.
Therefore, come to the office with a small supply of adult diapers or insert pads (ATTENDS or DEPENDS) that can be purchased at any drug store.
Once your catheter is removed it is recommended that you avoid caffeine, alcohol, and excessive fluid intake for 1-2 months as this can aggravate incontinence.
KEGEL EXERCISES
PELVIC MUSCLE EXERCISES TO IMPROVE BLADDER CONTROL (MALE)
Pelvic muscle exercises strengthen the group of muscles called the pelvic floor muscles. These muscles relax and contract under your command to control the opening and closing of your bladder. When these muscles are weak, urine leakage may result. However, you can exercise them and, in many cases,, regain your bladder control.
To achieve the best results when performing these exercises, imagine yourself an athlete in training. You need to build the strength and the endurance of your muscles. THIS REQUIRES REGULAR EXERCISE.
It is recommended that you start doing Kegel exercises six-eight weeks prior to surgery.
Begin by locating the muscles to be exercised:
- As you begin urinating, try to stop or slow the urine WITHOUT tensing the muscles of your legs, buttocks, or abdomen. This is very important. Using other muscles will defeat the purpose of the exercise.
- When you are able to stop or slow the stream of urine, you know that you have located the correct muscles. Feel the sensation of the muscles pulling inward and upward.
- You may squeeze the area of the rectum to tighten the anus as if trying not to pass gas and that will be using the correct muscles.
- Remember NOT to tense the abdominal, buttock, or thigh muscles.
Now you are ready to exercise regularly:
- After you have located the correct muscles, set aside time each day for three to four exercise sessions (morning, midday, and evening)
- Squeeze your muscles to the slow count of five. Then, relax the muscle completely to the slow count of five. The five second contraction and the five second relaxation make one “set.”
TIPS
- When your pelvic floor muscles are very weak, you should begin by contracting the muscles for only three to five seconds. Begin doing what you can and continue faithfully. In a few weeks, you should be able to increase the amount of time you are able to hold the contraction and the number of exercise sets you are able to do. Your goal is to hold each contraction for ten seconds, to relax for ten seconds, and to complete 25 to 30 Kegels three to four times per day.
- In the beginning, check yourself frequently by looking in the mirror or placing a hand on your abdomen and buttocks to ensure that you do not feel your belly, thigh, or buttock muscles move. If there’s movement, continue to experiment until you have isolated just the muscles of the pelvic floor.
- If you are unsure that you are contracting the correct muscles, at your next exam, ask your urologist to help you identify the proper muscle contraction.
- It is important to know that full control of urination may take even up to one year to return completely following surgery. Most men experience improvement within 3-6 months. By 6 months, 70% of patients are pad-free and 90% are pad-free at one year.
- Exercise your pelvic muscles regularly for a lifetime to improve and maintain bladder control.
- Pelvic muscle exercises also improve orgasmic function. Whether you are doing pelvic muscle exercise to improve or maintain bladder control or improve orgasmic function, or both, they must be done faithfully. Make them part of your routine.
FREQUENTLY ASKED QUESTIONS
1. How long is the operation?
The length of this operation may vary based on a patient’s weight, size of the prostate, and the presence of scarring around the prostate gland. In general, these cases can last anywhere between 2.5 to 3 hours.
2. Will I need a transfusion and do I need to donate blood?
Transfusions are rare with these minimally invasive techniques. This is one of the most significant advantages over open surgery as bleeding is drastically reduced as compared to open surgery with routinely only 100-200 cc of blood loss. Donation of blood is optional but not generally required nor recommended.
3. How much pain will I have after surgery?
Patients often require a small amount of intravenous and/or oral narcotic pain medication during their hospital stay.
4. How long is the hospitalization?
Hospitalization is usually 2-3 days with these minimally invasive robotic techniques. Patients are able to walk the following day under their own power.
5. How long will I have to have the bladder catheter?
Removal of the catheter will be dependent on the surgeon’s particular preference. In general, however, because of the excellent visualization offered by these minimally invasive robotic techniques a water tight connection between the bladder and urethra can be easily achieved allowing for safe removal of the bladder catheter within 1-2 weeks following surgery.
6. When can I return to normal activities?
In general, patients can take short walks and climb stairs after discharge and most patients can return to full activities by 3-4 weeks after surgery. However, urinary control and sexual function may take months and even up to a year or so to improve significantly, just as in open surgery.
7. What is my chance of urinary incontinence?
Most men experience at least some degree of stress urinary incontinence for example when sneezing or coughing. This generally improves with time and with vigilance in performing Kegel exercises. We have found that approximately 70% of men were dry at 6 months and 90% at 12 months following Robotic Radical Prostatectomy. Recent studies have shown early return to urinary continence after robotic radical prostatectomy.
8. What is my chance of erectile dysfunction?
The return of erectile function is perhaps the most difficult outcome measure to predict. Many factors are involved in the return to sexual function following surgery including age of the patient, having an active sexual partner, whether one or both nerve bundles were spared, and time since surgery. Studies have shown that in preoperatively potent men who underwent nerve sparing Robotic Radical Prostatectomy, approx. 50% of men (who had both nerve bundles spared) reported successful intercourse at 6 months and 72% at one year following surgery with or without the use of oral medications (e.g. Viagra or Cialis). Younger men appear to have a higher potency rate as compared to older patients at one year .
9. Will I need to follow up with the Urologist after my surgery?
Your first follow up appointment will be for catheter removal in 1-2 weeks following surgery. Following this, a PSA test at one month and office visit is recommended at 3, 6, 12 months and then typically annually thereafter.
10. When will the pathology results be available?
Once the cancerous prostate gland is removed it is thoroughly evaluated by the pathologists. They are able to identify the Gleason grade, location, and extent of the cancer. In general, these results are made available to the surgeon in 5-7 days.
11. Will I need further treatment following surgery for my prostate cancer?
Much of the decision on whether further treatment such as radiation or hormonal therapy is required will be based upon the pathologic stage of the cancer as well as the trend in PSA values following surgery. Most patients nowadays have early cancers detected by PSA screening and therefore are by and large curable with surgery. Therefore, most patients do not require additional therapy following surgery. But obviously each case is individualized.
