Prostate cancer is the second most commonly occurring cancer in men and the fourth most commonly occurring cancer overall. According to the recent data by ICMR, in India, the incidence rate of prostate cancer is reported as 9-10/100000 population which is higher when compared to Asia and Africa, but lower compared to the USA and Europe.
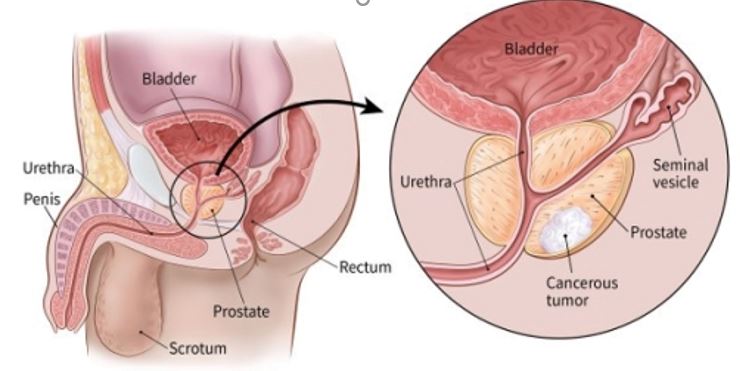
As the name suggests, it occurs in prostate — a small walnut-shaped gland in men that produce prostatic secretion, which is necessary to preserve vitality of sperm. This cancer is generally slow growing and the majority of men with low grade prostate cancer live for many years without symptoms and affecting survival of patient, in fact these patients die due to other illness rather than from prostate cancer.
Because of more awareness, regular health check ups and increased screening, most men are diagnosed at an earlier stage of prostate cancer and have a good chance of recovery. But, once prostate cancer begins to grow quickly or spreads, as in high grade disease, it is dangerous.
Causes/ Risk Factor
It’s still not known what causes prostate cancer, although a number of things can increase the risk of developing the condition. Cancer grows from cells which have acquired mutation or inherited mutation (familial cancer) in their genetic material. Familial prostate cancer occurs in men who have particular genetic mutations, such as genetic mutations seen in some families with breast and ovarian cancer. However, most cancer-causing genetic mutation occurs after birth.
There are some risk factors which may affect one’s chances of developing prostate cancer. These include:
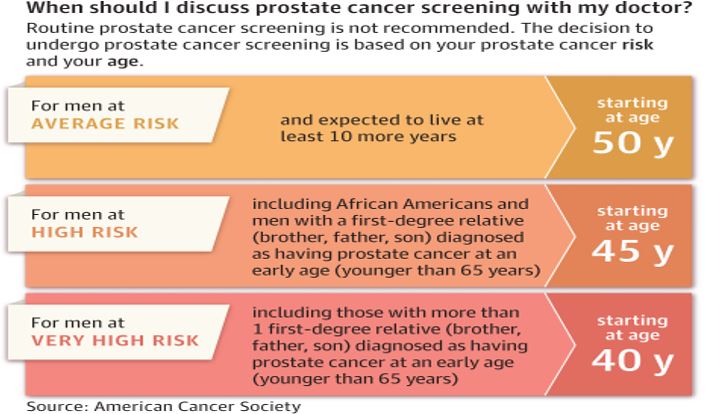
- Age – The risk rises as you get older, and most cases are diagnosed in men over 50 years of age.
- Ethnic group – prostate cancer is more common among men of African-Caribbean and African descent than in Asian men.
- Family history – having a brother or father who developed prostate cancer before age 60 seems to increase your risk of developing prostate cancer. Research also shows that mutations that lead to prostate cancer may be inherited. There is also an evidence that prostate cancer risk increase with having a close female relative with history of breast cancer. Genetic testing may be needed in these cases.
- Obesity – Some recent studies suggests that there may be a link between obesity and prostate cancer, and a balanced diet and regular exercise may lower your risk of developing prostate cancer.
- Geography: Prostate cancer is rarer in Asia, Africa, and South America.
- Smoking: People who smoke have a higher risk of developing prostate cancer and a poorer prognosis after diagnosis.
Symptom & Sign
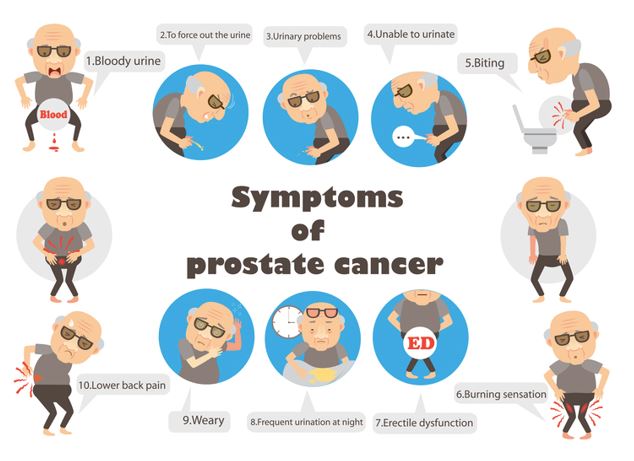
Prostate cancer does not cause any symptoms until it has reached a more advanced stage or significantly increased in size. It may then cause problems which may not be much different from benign (non cancerous) enlargement of prostate. These include
- Difficulty in starting to urinate or emptying your bladder
- A weak flow when you urinate
- Intermittent stream
- A feeling that your bladder hasn’t emptied properly
- Dribbling of urine after you finish urinating
- Needing to urinate more often, especially at night
- A sudden urge to urinate – you may sometimes leak before you get to the toilet.
- Urinary retention
- Blood in urine
- Renal failure, pain in lower abdomen, bleeding per rectum, new onset bone pain especially in back bone, weakness in both lower limb in advance prostate cancer.
Screening of healthy men for Prostate cancer : Should you be screened?
Screening for prostate cancer in men can be done with a simple blood test which is called Prostate-Specific Antigen (PSA) Blood Test. There are however recommendations as to which set of healthy individuals should be screened with PSA test to rule out prostate cancer. The recommendations vary according different bodies of guidelines but in nutshell are mentioned below.
Making and confirming the diagnosis
Before any treatment plan is prepared, a thorough investigation is done and as part of it below diagnosis tests are available for prostate cancer:
- Prostate-Specific Antigen (PSA) Blood Test : PSA may be elevated for reasons other than prostate cancer. Prostate conditions like benign prostate hyperplasia (BPH), infection, and inflammation can also raise PSA levels. These benign conditions should be ruled out/treated and PSA repeated usually after 4 weeks to avoid false interpretations.Historically, a PSA level of 4 ng/mL (nanograms per milliliter) or greater was generally regarded as high and raised concern for possible cancer. Some experts recommend even lower thresholds. A given PSA should be interpreted in light of a man’s age and other health factors to determine if a biopsy makes sense.PSA levels are used to determine the overall risk of an aggressive cancer. A PSA level of less than 10 ng/mL is considered to indicate a low risk of aggressive disease. A level of 10-20 ng/mL indicates intermediate risk and a level greater than 20 ng/mL suggests a high risk of cancer progression. However, PSA only provides part of your overall cancer picture and should be considered with other clinical factors (e.g. biopsy results, clinical stage, and prostate size)
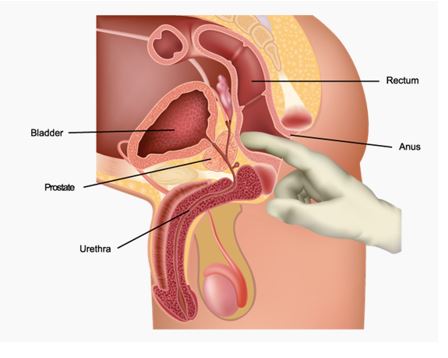
- Digital Rectal Exam (DRE) : During the DRE, a doctor inserts a lubricated, gloved finger into the patient’s rectum to feel for lumps, enlargements, or areas of hardness that might indicate prostate cancer. The procedure lasts for less than minute and, while uncomfortable, should cause no pain.
- Multiparametric Magnetic Resonance Imaging (MP-MRI): This produces cross-sectional slices of the body like a CT scanner, but it can also show slices (views) from several angles. MRI scans can be quite helpful in looking at prostate cancer. They can produce a very clear picture of the prostate and show whether cancer has spread outside the prostate into the surrounding structures( seminal vesicles or the bladder). This information can be crucial for your doctors in planning your treatment. Further the lesion in the prostate will be assigned a PIRADS score from 1-5 with 1 meaning non-cancerous to 5 meaning high likelihood of cancerous lesion. This helps us to decide on the need for prostatic biopsy as the next step in investigating your prostate lesion.
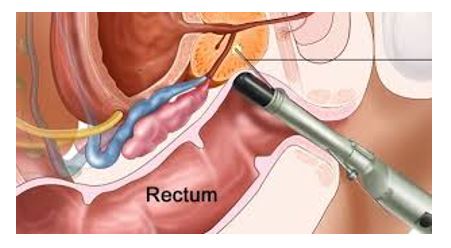
- TRUS (Transrectal Ultrasound) guided prostate biopsy
A Transrectal Ultrasound guided prostate biopsy (TRUS) is an investigation used to confirm the diagnosis of prostate cancer. In general, a TRUS prostate biopsy is performed in men with an abnormal PSA, a palpable abnormality on a digital rectal examination (DRE) or a rapidly increasing PSA level.An Ultrasound probe is inserted in the rectum and probe itself has a channel for inserting the needle so you may feel some pressure/stretch when the probe is inserted, but it is usually not painful. Usually 12 (sometimes more) prostatic tissue samples are obtained and the entire procedure lasts about 10 minutes. A local anesthetic can be used to numb the area and reduce any pain.
- Whole body PSMA PET CT Scan / Bone scan: It is a special kind of scan that is done after injecting a PSMA coupled ligand which is specific for prostate cancer cells. It helps define the spread/extent of prostate cancer elsewhere in the body. It is fast replacing the bone scan for high risk prostate cancer as bone scan tells about spread only in the bones.
WHAT ARE THE TREATMENT OPTIONS AVAILABLE?
Treatment of prostate cancer depends on the stage of disease
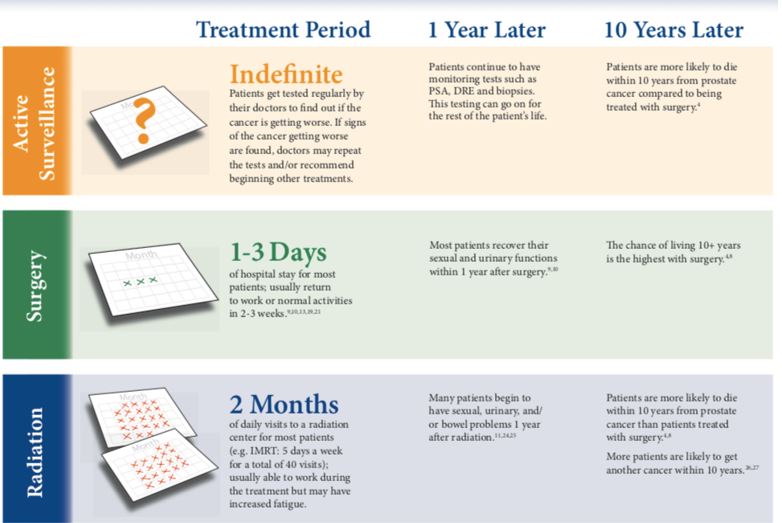
ACTIVE SURVEILLANCE (AS) / (WATCHFUL WAITING)

What it literally means ?
Active Surveillance means patient lives with prostate cancer without any active intervention. However, patient remains in close follow up and is tested regularly to see if it becomes worse.
How is patient followed up in AS
Patient undergoes a rectal exam and PSA blood test every 3-6 months, and a biopsy once a year. For each biopsy, your doctor will insert a thin needle into your prostate to remove about 12 tissue (or sometimes more) samples for testing.
Suitable Candidates/Benefits
- Patients with shorter life expectancy ( less than 10 years) because of age or other comorbidities
- Patients with slow-growing/ very low risk prostate cancer
- Avoids possible side effects of surgery, radiation or other treatments
- If treatment is needed in the future, tratment with curative intent possible.
Drawbacks
- Compliance for close monitoring is needed.
- As compared to surgery, patients on AS are more likely to die within 10 years from prostate cancer
- Regular biopsies are needed which can result in increased chance of erectile dysfunction
- Cancer may spread outside the prostate in the meantime.
- May miss the chance for curative treatment in future if cancer spreads or if the patient developIf treatment is needed in the future, you may be at an age when it’s more diffcult to tolerate.
- Many a times, (approximately 35-40%) prostate cancer can be undergraded (thought to be slow- growing when it is actually fast-growing and of higher risk)
SURGERY (PROSTATECTOMY)
The cancerous prostate gland along with surrounding tissues (mostly including lymph nodes) is removed by a surgery. The removed gland and surrounding tissue test results will let your doctors know how much cancer you had, and if it was all removed.
Modalities of surgery
- Now a days, surgery is performed in Robotic-assisted manner (minimally invasive) is with a few small incisions/cuts);
- Other Traditional mehods include laparoscopic surgery (minimally invasive with a few small incisions) or open surgery (with a large incision)
Advantages
- The main advantage of radical prostatectomy is that when skillfully performed, it offers the possibility of cure with minimal collateral damage to surrounding tissues.
- Further, it provides more accurate tumor staging by pathologic examination of the surgical specimen.
- Treatment failure/recurrence of disease is more readily identified.
- The postoperative course is much smoother than in the past.
- The hospital stay is usually 1 to 3 days, and operative mortality is rare in the modern era.
- Moreover, radical prostatectomy significantly reduces local progression and distant metastases and improves cancer-specific and overall survival rates compared with watchful waiting.
- Some patients with tumor recurrence after radical prostatectomy can be salvaged with potentially curative postoperative radiotherapy.
Disadvantages
- The potential disadvantages of radical prostatectomy are the necessary hospitalization and recovery period. This has reduced with the advent of Robot assisted surgery as hospitalization is short and recovery is much faster.
- Risk for erectile dysfunction and urinary incontinence. However, erectile dysfunction and rectal complications are less likely with nerve-sparing surgery than with radiotherapy, and good treatment options are available for both urinary incontinence and erectile dysfunction. Most patient can control their urine and recover sexual function over period of few months.
Benefits of da Vinci® Robotic Surgery
Surgery for prostate cancer is best done robotically now which is the standard of care. When available, da Vinci Surgery offers the following potential benefits compared to open surgery:
- Better cancer control,
- Faster return of erectile function
- Better chance for return of bladder control (urinary continence)
- Less blood loss and less need for blood transfusion
- Less pain
- Lower risk of complications/wound complications
- Shorter hospital stay and fewer days with catheter
- Faster recovery and return to normal activities
RADIATION THERAPY (RT)
What is radiation therapy for prostate cancer ?
A radiation oncologist will try to kill the cancer cells using high-dose radiation to the prostate, but will not remove the prostate.
Types of RT
- EBRT (external beam radiation) : Radiation from a source outside the body.
- Brachytherapy (radioactive seeds placed inside the prostate)
- IMRT (intensity-modulated radiation therapy) IGRT (image-guided radiation therapy)
- Other types of external beam radiation (EBRT)
Advantages
- Good chance for a cure for appropriate patients
- No hospital stay and few, if any restrictions to your activites after treatment
- May be used as an adjuvant treatment after surgery if cancer has spread outside of the prostate
Disadvantages
- More likely to die within 10 years from prostate cancer with radiation compared to surgery
- Increased fatigue during long treatment – usually 2 months (upto 40 separate treatment sessions)
- Urinary and bowel problems could last for years and sexual potency tends to get worse over time
- Prostate can move during treatment and cause radiation to hit other nearby tissues/organs and you are more likely to have another cancer.
- Very difficult to treat if cancer returns
Potential side effects of external beam radiation therapy for prostate cancer may include:
- Frequent urination.
- Difficult or painful urination.
- Blood in the urine.
- Urinary leakage.
- Abdominal cramping.
- Painful bowel movements.
- Rectal bleeding.
- Rectal leaking
- Fatigue
- Sexual dysfunction, including diminished erectile function or decrease in the volume of semen
- Skin reactions (similar to a sunburn)
- Secondary cancers in the region of the radiation
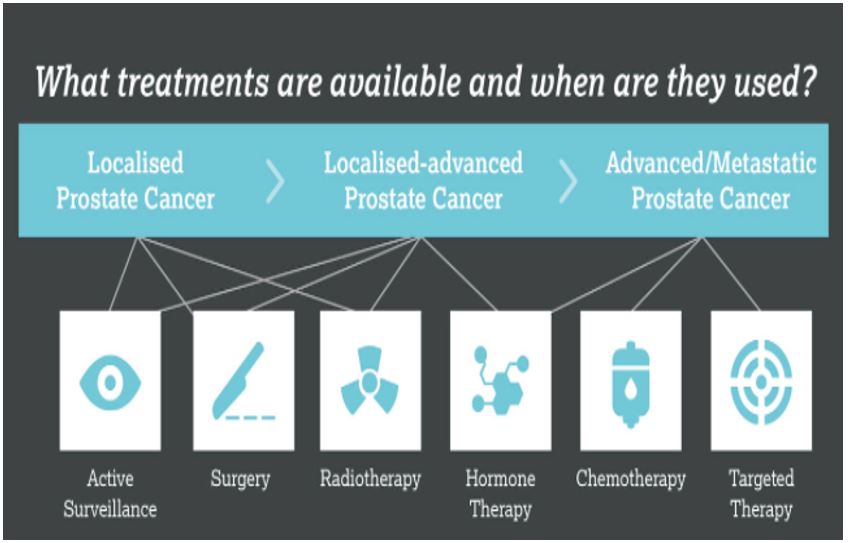
Localised Carcinoma Prostate : Treatment options at a glance
TREATMENT OPTIONS FOR ADVANCED/METASTATIC PROSTATE CANCER(WHEN CANCER HAS SPREAD TO DISTANT ORGANS IN BODY)
Multiple treatment options are available which may provide a long term control along with reasonable quality of life in patients of prostate cancer even when the disease has spread to distant organs. The overall result of the treatment however depends on the burden of disease in body.
Hormone Therapy
Hormone therapy is also called androgen deprivation therapy (ADT) or androgen Suppression therapy. Primary hormone therapy [androgen deprivation therapy or ADT] is part of the standard of care for advanced or metastatic prostate cancer and many a times given along with radiation therapy for localized or locally advanced disease. The aim is to reduce levels of male hormones, called androgens, in the body, or to stop them from affecting prostate cancer cells.
Achieving castrate levels of testosterone is the target as testosterone serves as the main fuel for prostate cancer cell growth. Androgen deprivation therapy causes sharp reductions in PSA as majority of prostate cancer cells die. However some cells may escape and become Castrate resistant prostate cancer (CRPC) and hence may need second or third line therapy.
There are several types of hormone therapies that are used to treat prostate cancer:
- Medical Castration: Injectible Hormone (Androgen Deprivation) Therapy in which monthly or three monthly or six monthly injections are given subcutaneously or intramuscularly . The choice of injections depend on the patient comorbities and side effect profile. Cost is the main downside and surgical castration may in indicated in appropriate patients.
- Orchiectomy (Surgical Castration) : Bilateral orchiectomy is the surgical removal of both testicles in order to achieve castrate levels of testosterone in the blood. It is indicated for metastatic disease as an alternative to injectible hormonal therapy for locally advanced or metastatic disease especially if patients life expectancy is less than 10 year.
Chemotherapy
Chemotherapy is sometimes used if prostate cancer has spread outside the prostate gland and hormone therapy isn’t working and even as primary therapy in fit patients.
Palliative surgery (for non-curable, metastatic prostate cancer):
- Transurethral Resection of Prostate (TURP)
This operation is more commonly used to treat men with non-cancerous enlargement of the prostate – BPH. When it is used for prostate cancer, it is palliative, which means it is done to relieve symptoms (urinary retention, need of repeated catheterisations) and not to cure it.
Post-treatment care:
Regardless of which treatment option you choose, you will be under regular follow up to see if your cancer recurs or spreads further. Follow up will include regular visits and investigations such as PSA and PSMA PET CT. Most doctors recommend PSA tests about every 3-6 months for the first 5 years after treatment, and at least yearly after that.

